Medical Coding Jobs: The medical field is rife with complexities that require astute attention. Besides diverse medical procedures, healthcare companies also need to handle adjacent activities like documentation, insurance form processing, medical coding and billing, etc.
But, tasking medical professionals with such back-end operations when they are already overwhelmed with providing quality care can lead to medical coding errors, which can wreak havoc on the entire healthcare establishment with issues like claims process delays, revenue loss, incorrect patient care, etc. Fortunately, you can take measures to prevent them and improve process efficiency with the help of medical billing and coding services professionals. This blog describes these preventive measures, their implementation, and the many benefits they offer.
Table of Contents
The Common Medical Billing and Coding Errors
- Report Misinterpretation
Report misinterpretation is when a coder incorrectly notes down observations made by the physician. It is caused by numerous factors. It results in wrong coding and rejection of claims by the insurer. Patient health records containing wrong information due to this error can lead to possibly fatal consequences. It also increases costs to both patients and administrators as the patient may needlessly occupy a bed awaiting claim settlement.
- Standard Incompatibility
Medical coding and billing processes are dictated by global and local standards. The WHO’s International Classification of Diseases, Tenth Revision (ICD-10) is an example of a global standard. An example of a local or regional code standard is the U.S.A.’s Current Procedural Terminology (CPT). A coder should work according to applicable standards. Otherwise, it leads to incompatibility down the document processing pipeline.
- Unbundling and Under/Upcoding
These types of medical coding errors are purposeful and fraudulent. Under coding happens when less-expensive medical services are coded in place of those performed. Upcoding or Overcoding refers to coding-in procedures which are more expensive than the actual ones performed. Unbundling also works like Upcoding, where medical procedures get charged separately.
- Missing Information/Documentation
Insufficient or missing information may result in coders documenting things wrongly.
They may also not find the needed medical personnel for a consultation about difficult-to-understand information. Such erroneous documents will get rejected by the insurer, causing confusion and delays.
- Other Simple Errors
Other commonly occurring errors are incorrect patient data entry (such as name, age, sex, weight, etc.), false insurance provider data, wrong medical professional data (such as name, address, and contact information), confusing use of codes (like using excessive or insufficient digits, wrong modifiers, etc.), omission of procedural codes, and bill duplication.
Tips To Prevent Medical Coding Errors
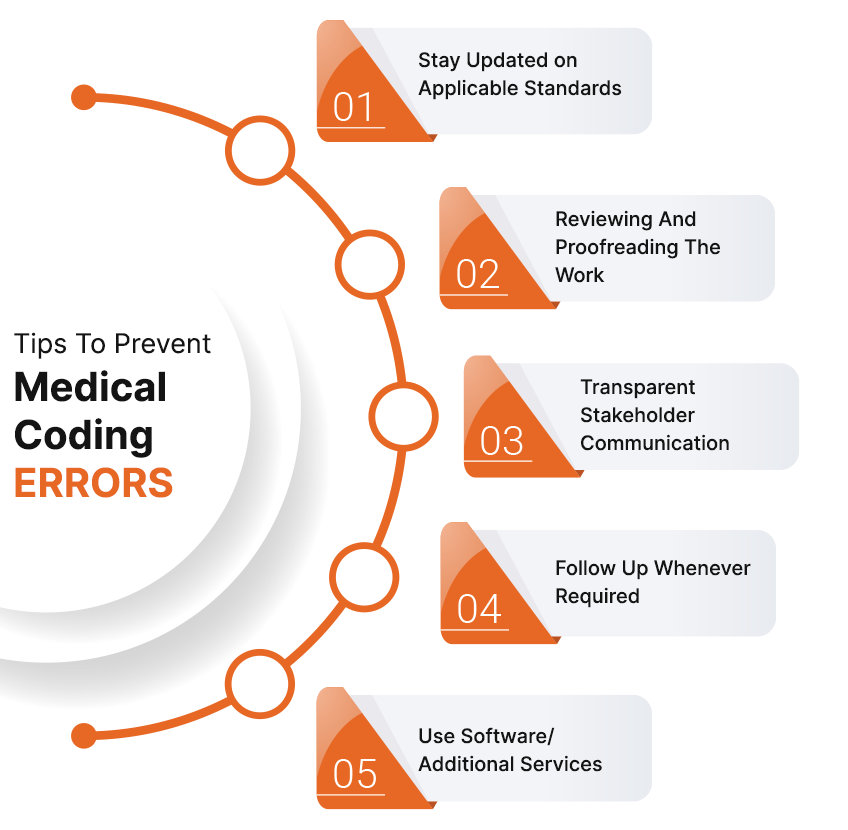
- Remaining Updated On Applicable Standards
Remain vigilant about coding and billing standards updates. For instance, ICD-10 is updated annually, and those changes must be incorporated into your coding as quickly as possible. Regularly check to see if your membership in any coding associations, such as the American Academy of Professional Coders (AAPC) or American Health Information Management Association (AHIMA), requires reapplication or review.
- Reviewing And Proofreading The Work
Reviewing completed work helps you identify and rectify errors before the documents proceed to the next stage. Besides medical errors, you can also catch grammatical ones that could lead to document interpretation issues. Check for the addition or omission of digits, lack of reporting of incorrect code, patient and medical service provider information, the standard used to code, date and time of entry, and the like.
- Communicating Clearly With Concerned Stakeholders
Lack of communication between stakeholders causes medical coding errors and process delays. Coders may have to assume certain information, hurting accuracy. Hurriedly written notes can also be difficult to interpret, increasing the chances of errors. The lack of consultation can cause accuracy issues too. Therefore, you should maintain clear communication with all applicable personnel, including scheduling consultation appointments.
- Follow Up Whenever Required
People can sometimes forget their assigned tasks. The subsequent delays and errors can disrupt multiple processes despite your best efforts to the contrary.
Thus, it’s best to regularly follow up on all concerned parties. Verify where in the pipeline your documents are and their contents accuracy too. Check if claims were paid correctly and on time. You must include an explanation of benefits (EOB) made by the payer whenever a claim has been rejected or denied.
- Use Software/Additional Services
Medical coding and billing require multitasking as many variables need to be accounted for throughout the process. Reducing variable uncertainties to the maximum extent improves accuracy and overall efficiency.
Additional support services like medical data entry, data cleansing services, and the latest software can improve data quality. It makes the company’s database reliable and intelligible enough to perform all sorts of processes using it.
Why You Should Outsource Medical Coding and Billing
One of the best solutions to your coding and billing problems is to employ dedicated medical billing and coding services as professional agencies can handle the challenges of this job. They can offer your organization a bevy of benefits that go a long way in improving the bottom line and efficiency, like:
- Lower Cost
The economies of scale and currency exchange help reduce costs compared to in-house operations.
- Quick Turnover Times
Experienced personnel, dedicated workflows, sufficient resource availability, capable infrastructure, easy scalability, etc., contribute to reduced output times.
- Access To Expertise
Medical coding outsourcing agencies always have experts ready to work on your tasks, saving you time in finding the right kind of professionals for the job. It also saves time and costs.
- Accurate Compliance
Outsourcing agencies keep themselves updated about the latest compliance requirements for all applicable tasks. You no longer need to worry about related issues.
- Better Customer Support
Having accurately coded information means being able to better support your patients, i.e., your customers. This develops more trust in them about your healthcare center and improves brand image.
In Conclusion
Coders have to continuously adapt to the ever-changing healthcare industry while maintaining output quality. The problems prevented by taking such corrective measures, including the use of additional professional agencies like medical coding services, medical billing services, etc will help save money and the facility’s reputation along with patients’ lives. Hopefully, this blog can be of help in this safeguarding journey.
Pranay, a coding maestro weaving digital magic with Dot Net,Angular. With 4+ years in web development,he specialize in crafting seamless solutions. Beyond coding, Pranay is a wordsmith, passionate about sharing insights through guest posts. Whether crafting code or narratives, he bring creativity and precision to every project. Connect to explore his coding journey and delve into the world where tech meets storytelling .follow us on X